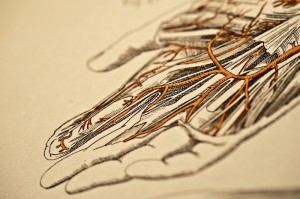
Reconstructive hand surgery corrects many different functional and cosmetic conditions. Rheumatoid reconstruction of the hand can repair joint deformities caused by rheumatoid arthritis. These procedures help relieve the pressure and pain and cosmetic deformities associated with this common hand disorder.
Typical hand difficulties associated with Rheumatoid arthritis include nerve compression/numbness leading to carpal tunnel syndrome, severe arthritis and deformity, tendon rupture and swelling, and cosmetic deformities of the fingers that affect function.
What is rheumatoid arthritis of the hand?
Rheumatoid arthritis is considered a systemic disease, as it can affect many different areas of the body. The joints and soft tissues become inflamed, swell, and do not function smoothly. Around two thirds of people with rheumatoid arthritis have hand and wrist problems.
With this chronic form of arthritis, the cells that lubricate and line the joints are affected. The joint cartilage and bones erode and the ligaments and tendons stretch out, making the hand and wrist look deformed. There are many classic features of hand rheumatoid arthritis. These include firm nodules along the fingers, angulation or collapse of the fingers, soft lumps on the back of the hand that moves as the fingers straighten, and deformities of the fingers.
What are the different surgical options?
There are many non-surgical and surgical options involved with rheumatoid reconstruction of the hand. Many of the decisions require complex decision making about ultimately what will benefit the patient most. Fortunately, there are many newer medications that have reduced the need for advanced surgery in most patients. However, some patients continue to worsen in pain, function and cosmetics to still require traditional operative treatments.
Typical surgeries include Tendon Repairs and Reconstructions, Joint repairs/fusions or joint replacements, nerve releases, and removal of inflamed tissues.
When is joint replacement surgery the best surgical option?
A joint replacement procedure of the wrist, or fingers is an innovative option for treating arthritis of the hand in in well-selected patients with rheumatoid arthritis. Joint replacement surgery can provide increased finger and wrist, range of motion, improve hand function, and most importantly, pain relief. This surgery involves replacing a worn out joint with an artificial one. The new joint is most often composed of silicone rubber, metal and plastic or the patient’s own tissue, which pads the worn out bone ends.

 We see many patients who have lumps and bumps in their hand that are painful, growing, affect function, and are often worry some for the patient due to the concern for cancer. If you are concerned about a hand tumor, wrist mass, or finger cyst, you should schedule a consultation to put your mind at ease with a diagnosis and to discuss treatments available.
We see many patients who have lumps and bumps in their hand that are painful, growing, affect function, and are often worry some for the patient due to the concern for cancer. If you are concerned about a hand tumor, wrist mass, or finger cyst, you should schedule a consultation to put your mind at ease with a diagnosis and to discuss treatments available.